In First-of-Its-Kind Trial, Scientists Use CRISPR to Treat Cancer
 isbscience.org/news/2022/11/10/in-first-of-its-kind-trial-scientists-use-crispr-to-treat-cancer/
isbscience.org/news/2022/11/10/in-first-of-its-kind-trial-scientists-use-crispr-to-treat-cancer/Scientists for the first time have used CRISPR to substitute a gene to treat patients with cancer. The remarkable findings were published in the journal Nature and presented at the Society for Immunotherapy of Cancer (SITC) 2022.
Cancer treatments, while targeted at cancer cells, can often also impact healthy tissues and lead to serious side effects. The reported approach first identifies T cells that specifically recognize and kill an individual patient’s tumor cells. T cells are a type of immune cell, and the cells in question kill tumor cells when they encounter specific genetic mutations arising from the cancer. However, there often aren’t enough of those cells. By CRISPR editing other T cells from the patient with the same cancer recognition motifs, the approach is designed to build a large army of cancer fighting cells, which are then infused back into the patient, thus greatly amplifying that natural anti-tumor response.
CRISPR gene editing, which is commonly used to knock-out specific genes, was also developed here to knock-in the critical genes for enabling T cell recognition of the tumor. This new approach avoids the use of retroviruses, and, by doing so, greatly shortens the time required to manufacture a personalized cell therapy for cancer.
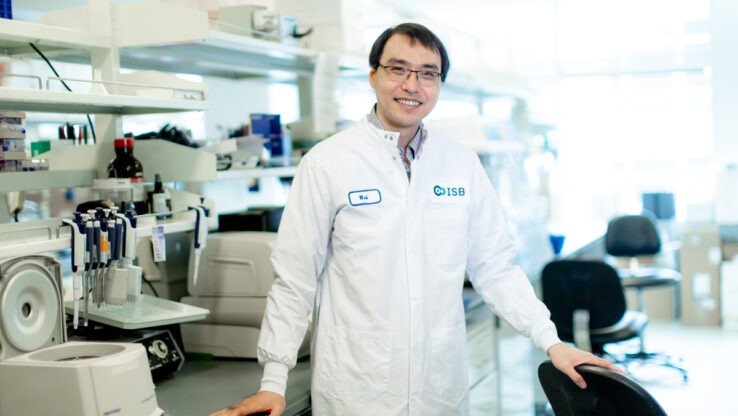
“This is a tremendous step forward for personalized cancer treatment,” said ISB President Dr. Jim Heath. “It is heartening to see our early work of isolating immune receptors that can recognize cancer mutations be used in such meaningful and groundbreaking ways. This is a truly exciting advancement in cancer treatment.”
PACT Pharma – founded based upon work pioneered by Heath and his collaborators, UCLA Professor Dr. Toni Ribas and Caltech Professor Dr. David Baltimore – developed the therapy approach, and then harnessed it to treat 16 patients. The primary objective of the early stage clinical trial was to show that the treatment was safe to patients, but the researchers also found that the engineered T cells did, in fact, home in on the patient tumors.
“This is a leap forward in developing a personalized treatment for cancer,” Ribas said. “The generation of a personalized cell treatment for cancer would not have been feasible without the newly developed ability to use the CRISPR technique to replace the immune receptors in clinical-grade cell preparations in a single step.”
You can learn more about this work by clicking play on the video above, or by going here.
You can also learn more about the immune system by watching the following video featuring ISB Assistant Professor Dr. Jennifer Hadlock.