Cancer Detection: A Systems Biology Approach
 isbscience.org/news/2014/05/12/cancer-detection-a-systems-biology-approach/
isbscience.org/news/2014/05/12/cancer-detection-a-systems-biology-approach/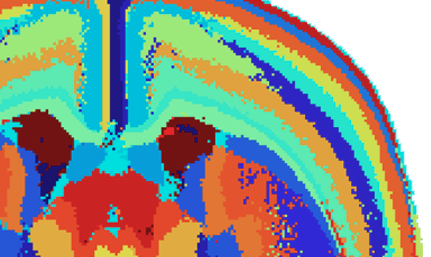
By Martin Shelton
ISB Editorial Board Member
With the exception of cancers of the skin, mouth, and blood, it is difficult to detect cancer by sight or with a routine health screen. The natural variety that exists at the cellular level — even within cells of the same type — challenges our ability to differentiate healthy tissue from diseased. This variety, what biologists call heterogeneity, means that equally healthy cells may look quite different from one another.
Further, cancers typically don’t manifest symptoms until later stages of progression, which decreases the usefulness of symptoms in early detection. In viral infections of the respiratory system, for example, the initiating event is quickly followed by symptoms such as a runny nose, cough and fever. In contrast, the emergence of the first cancerous cell is so far removed in time from detectable symptoms — a tumor “lump” in breast tissue, a sudden loss of cognition due to a brain lesion, a broken bone due to metastasis — that the connection isn’t always evident.
This is part of a series on ISB's systems biology approach to cancer research. Read the introduction or about
cancer stratification and cancer treatment.
If scientists had samples taken from patients before and after the initiating event in cancer, they would be better able to study and understand the transition from health to disease. More importantly, they would be able to study the changes in the measurable biological characteristics (biomarkers) that are crucial to early detection. Understanding the subsequent progression of the disease also informs the development of better drugs and clinical tests, eventually improving detection, treatment and the monitoring of treatment efficacy.
"Understanding the transition, and more importantly, the measurable biological characteristics — biomarkers — that change during this transition, is the key to early detection."
How ISB Applies A Systems Approach to Detection
Prion Disease
In one of ISB’s hallmark studies, an international team of researchers, led by Daehee Hwang, Inyoul Lee, Hyuntae Yoo and Lee Hood at ISB, applied a systems approach to the study of prion diseases, a class of neurodegenerative diseases that includes Creutzfeldt-Jakob Disease and Mad Cow Disease, and showed that they could diagnose the disease well before symptoms developed using a blood test. Using mice infected with prions as model organisms and network analysis, they reduced a list of ~7400 genes that were expressed at a different level in infected mice than in healthy mice to 300 genes related to prion-induced neurodegeneration. To put this in context, 7400 genes represents almost one-third (1/3) of the total number of protein coding genes in the mouse genome. Nearly 200 of the 300 “differentially expressed” genes could be mapped to one of four major networks that were involved in the disease process, and which became perturbed in a sequential order as the disease progressed. The remaining 100 differentially expressed genes mapped to six smaller networks that were not previously known to play a role in the disease. When all 10 networks were examined collectively, they explained essentially all aspects of the disease-associated neurodegeneration, including the dynamics of its progression. Remarkably, some of these genes encode proteins that get released from brain cells into the blood. Similar to their corresponding genes, these proteins were expressed at different levels depending on the health of the mouse. Thus, by measuring their levels in the blood, the researchers were able to diagnose infected mice a full 10 weeks before symptoms appeared and then follow the disease’s progression from start to finish. This study showed the power of applying systems biology approaches to the study of human diseases. Now we are applying the same approaches to cancer.
Brain Cancer
The most common types of brain cancers are astrocytomas, which are malignant tumors that arise from a class of brain cells called astrocytes. The tumors can be classified by their level of malignancy on a grade scale from I – IV, with Grade I representing benign, non-cancerous tumors, and Grade IV (high-grade astrocytomas) representing highly invasive, very aggressive malignant tumors. These Grade IV astrocytomas are also referred to as glioblastoma multiforme, or GBM for short. As the disease progresses, the overall survival rate decreases dramatically from 8-10 years for patients diagnosed with Grade II tumors to 9-12 months for those diagnosed with GBM. Unfortunately, the majority (~70%) of low- and medium-grade astrocytomas go undetected only to emerge, without clinical warning, as GBM. In addition to the obvious tragedy this represents for patients and their family members, the dismally low detection rate of lower grade astrocytomas also means that researchers seeking to understand the progression of this disease are severely handicapped, lacking the crucial tissue samples from the stages that lie between health and advanced disease.
To address this challenge and gain insight into the mechanisms underlying the GBM development, researchers from across the country, including Burak Kutlu, Rhishikesh Bargaje and Lee Hood at ISB, used a group of mice that had been genetically modified to begin developing astrocytomas upon exposure to a specific chemical. Because the researchers would be able to control the disease initiating event, they could monitor both the transition from health to disease and the progression of the tumor from low-grade to high. This proved to be a powerful model for studying GBM development. Focusing in on three major networks that had previously been shown to be affected in GBM patients, the researchers were able to determine the exact order, from tumor initiation through progression to full-blown GBM, in which the networks malfunctioned. More specifically, they now know which of the three networks to examine for identifying biomarkers of early disease.
Lung Cancer
For a patient, determining whether a growth is benign can be as important, and as challenging, as detecting cancer. Often, diagnosis of a growth requires an invasive and costly surgical biopsy. Lung nodules are growths that, if malignant, may lead to lung cancer. A whopping 80 percent of patients who are diagnosed with having lung nodules endure invasive biopsies that turn out to be unnecessary. Researchers at ISB and Integrated Diagnostics (Indi is an ISB spinout) designed a blood test consisting of a panel of 13 biomarkers that will assist in identifying benign lung nodules. It has a 90% negative predictive value (NPV), which means that if the test calls the nodule benign (i.e. the result is negative), 90% of the time the test is correct. Indi currently is in the process of commercializing the diagnostics test, which ultimately will save patients from unnecessary — and expensive — invasive procedures.
Technology Innovation
Understanding the transition from health to disease and transforming knowledge into clinically actionable biomarker tests are major drivers in ISB’s contributions to cancer research. To that end, ISB has developed computational tools as well as databases that are open-access to the cancer research community. Two examples: The Baliga lab at ISB developed the Cancer miRNA Regulatory Network to identify clinically relevant proteins and the miRNA molecules that regulate them for cancers affecting about 20 organs. The Moritz lab at ISB designed the SRMAtlas, which offers researchers rigorously validated mass spectrometry assays for detecting and measuring proteins, which is an important tool to identify biomarkers
About Dr. Martin Shelton: Martin is a postdoc in the Hood lab at ISB. He is a member of ISB's Editorial Board.