For Cancer Cells, There Is More Than One Path to Drug Resistance
 isbscience.org/news/2020/05/11/cancer-drug-resistance/
isbscience.org/news/2020/05/11/cancer-drug-resistance/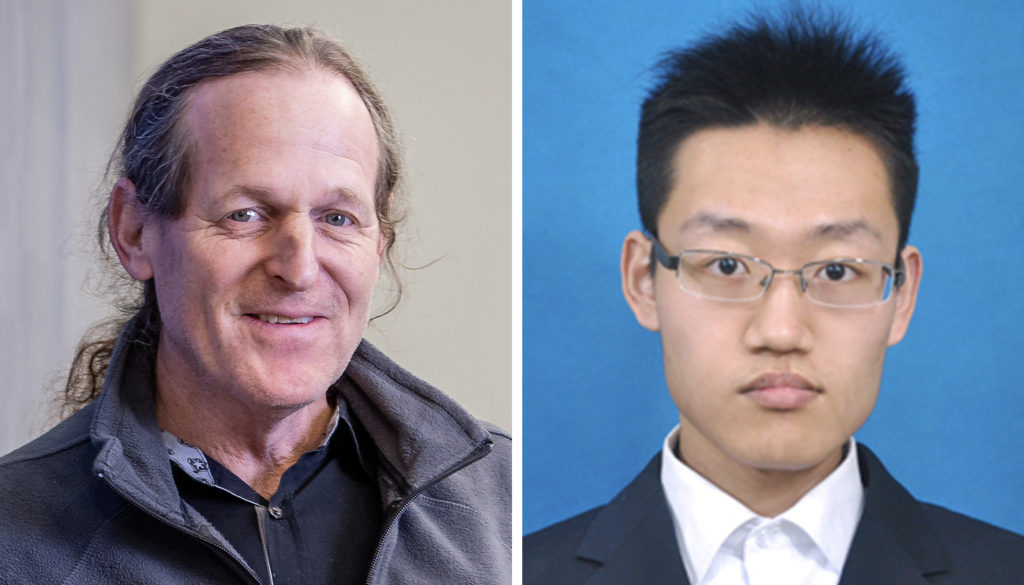
Co-corresponding author and ISB President Dr. Jim Heath and co-lead author Dr. Yapeng Su.
As the global cancer burden continues to rise, scientists are staring down a well-known and perplexing challenge: a cancer cell’s ability to become drug-resistant despite our best treatments.
For the past several years, researchers have been digging into the genome to look for any new mutations that cancer cells obtain during treatment that may cause resistance. This is called the genetic mechanism of resistance, which is also the dogma in the field of drug resistance. While genetic mechanisms are important, it usually takes a long time for tumor cells to find the right mutation to enable resistance.
Recently, researchers have realized that cancer cells can become resistant without the need to gain new mutations, and such non-genetic mechanisms of resistance are occurring much faster — sometimes just a few days after drug treatment. These researchers have been trying to understand the biological mechanisms that change cancerous cells from drug-sensitive to drug-tolerant without a change in the genome.
In findings published in the journal Nature Communications, researchers from ISB, Caltech, and several other institutions show that cancer cells can take more than one path to reach a drug-resistant cell state. “This is new and scary to hear,” said Dr. Yapeng Su, co-lead author. Su was a graduate student in ISB’s Heath Lab and Caltech’s Baltimore Lab while conducting this work, and has since earned his PhD.
Researchers worked with mutant melanoma cancer cells (BRAF600E) as a model due to the cell line’s rapid drug-responsive-to-drug tolerant transition against targeted inhibitors.
Past scientific experiments have shed some light on the mechanisms of drug tolerance at the cellular level. However, those studies compared drug-tolerant and drug-sensitive cells at the bulk level without single-cell resolution, or did not provide a detailed time-resolved characterization of the trajectories connecting those two states.
“It is important to analyze cancer cells one at a time rather than taking an average to really see and block all possible paths that cancer cells can take to escape drug inhibition in order to fully prevent drug resistance,” Su said.
Independent Paths Cancer Cells Can Take to Drug Resistance
Considering the importance of phosphorylated-protein signaling and metabolic changes that occur in the early stages of drug adaptation, Su and his colleagues characterized the transition using integrated single-cell functional proteomic and metabolic assays designed to broadly sample proteins and metabolites associated with selected cancer hallmarks and cell state-specific processes. “Being able to integrate information across different biological layers is key, as we will have less chance to miss something important,” Su said.
The resulting comprehensive dataset is huge and requires sophisticated data science approaches to gain critical information from it. In the study, a machine learning-based dimensional reduction was synergized with a thermodynamics-inspired information-theoretic analysis to digest the big data, which enabled clear visualization of the tremendous time-series single-cell data as two distinct paths connecting between drug-naive and drug-tolerant states.
“Clearly, there may be two independent paths cancer cells can take to become resistant,” Su said.
Further experiments confirmed whether these paths constituted independent cellular trajectories. The researchers even found that isogenic tumor cells can undertake different, independent trajectories to drug tolerance. And the two trajectories are associated with distinct signaling and metabolic networks that are independently druggable.
These findings highlight the importance — and challenge — of finding drug combinations that can prevent the cancer cells from transitioning into a drug-resistant state.
“This work challenges the current paradigm of targeted inhibitor resistance development, and offers new concepts for assessing the value of combination therapies,” said ISB President Dr. Jim Heath, who is co-corresponding author of the paper.
This work was a collaboration between ISB, Caltech, Stanford, The Hebrew University, Chinese Academy of Medical Sciences and Peking Union Medical College, and Suzhou Institute of Systems Medicine.