Molecular Biologist Dr. Sui Huang: We Should All Be Wearing Masks
 isbscience.org/news/2020/04/01/we-should-all-be-wearing-masks/
isbscience.org/news/2020/04/01/we-should-all-be-wearing-masks/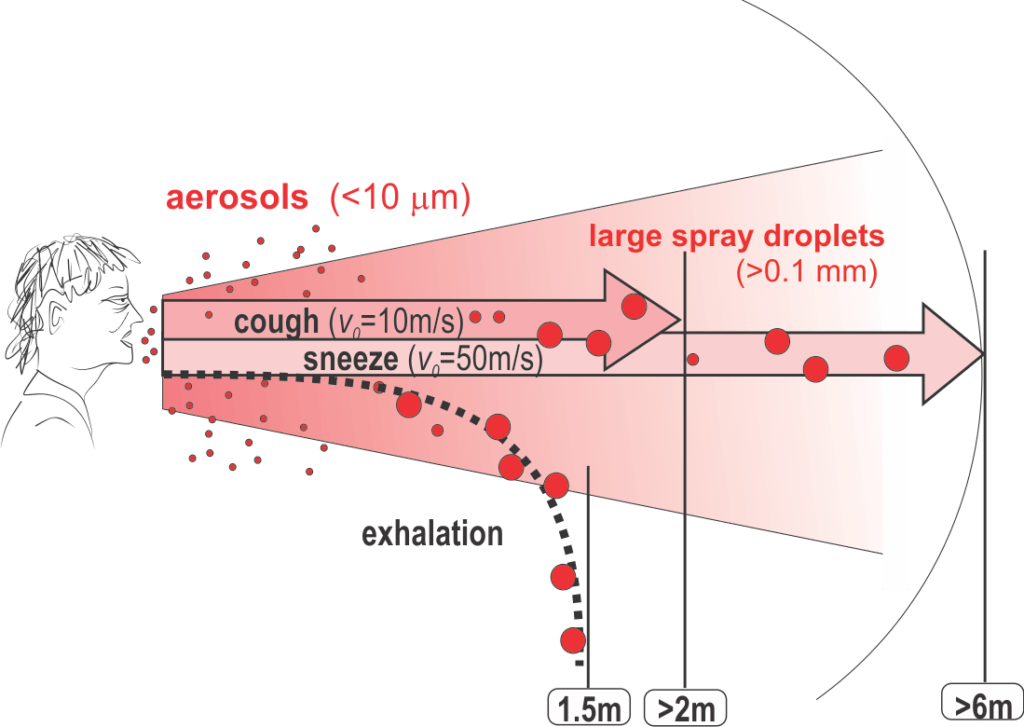
Droplets larger than aerosols, when exhaled, evaporate or fall to the ground less than 1.5 m away. When expelled at high velocity through coughing or sneezing, especially larger droplets, can be carried by the jet more than 2m or 6m, respectively, away.
© Dr. Sui Huang, ISB
ISB Professor Sui Huang, MD, PhD, was one of many experts calling on public officials to rethink official recommendations in the U.S. and other western countries and to embrace wearing masks amid the coronavirus pandemic.
Huang, a molecular biologist and ISB professor, was a powerful voice contending that masks are an effective tool to stop the spread of COVID-19. Huang had called initial guidelines from the CDC and other public health agencies “unfortunate,” as they swept aside a potentially powerful measure that can help “flatten the curve.”
Huang wrote a March 26 article (COVID-19: Why We Should All Wear Masks — There Is New Scientific Rationale) that has been viewed millions of times on Medium, and he has since discussed that rationale in a video Q&A.
“Masks are very important and effective,” Huang said. “Even if you act out of fear and out of a sense to protect yourself, you actually also protect others. It’s a bidirectional protection. We have a public incentive constellation that the CDC has missed.”
Watch the Video Q & A
Huang also cited recently published data in the journal Nature that shows the nose and throat is where the virus lands, where the body’s receptors for virus docking are, and where the virus replicates. This important discovery by a German group suggests that transmission occurs mostly via large droplets and less via those fine aerosols that can end up deep in the lung. Thus, even a surgery mask or do-it-yourself (DIY) cloth mask will act as an effective barrier. Higher-grade N95 masks aren’t needed to block the large spray droplets that come from the nasopharynx. (N95 masks filter out 95 percent of small airborne particles. They are necessary to block these tiny aerosolized droplets that reach the lower lungs, but are overkill for the larger droplets that originate from and land in the upper respiratory system.)
If the “respiratory etiquette” of sneezing into your elbow is protective, then masks should be protective, Huang said. “Any physical barrier should be helpful,” he said. “When empirical evidence is lacking, we should trust measures based on common sense, plausible mechanisms — especially when costs are minimal.”