New Method to Detect, Analyze Rare T Cells Another Step Toward Personalized Cancer Vaccines
 isbscience.org/news/2019/09/04/new-method-to-detect-analyze-rare-t-cells-another-step-toward-personalized-cancer-vaccines/
isbscience.org/news/2019/09/04/new-method-to-detect-analyze-rare-t-cells-another-step-toward-personalized-cancer-vaccines/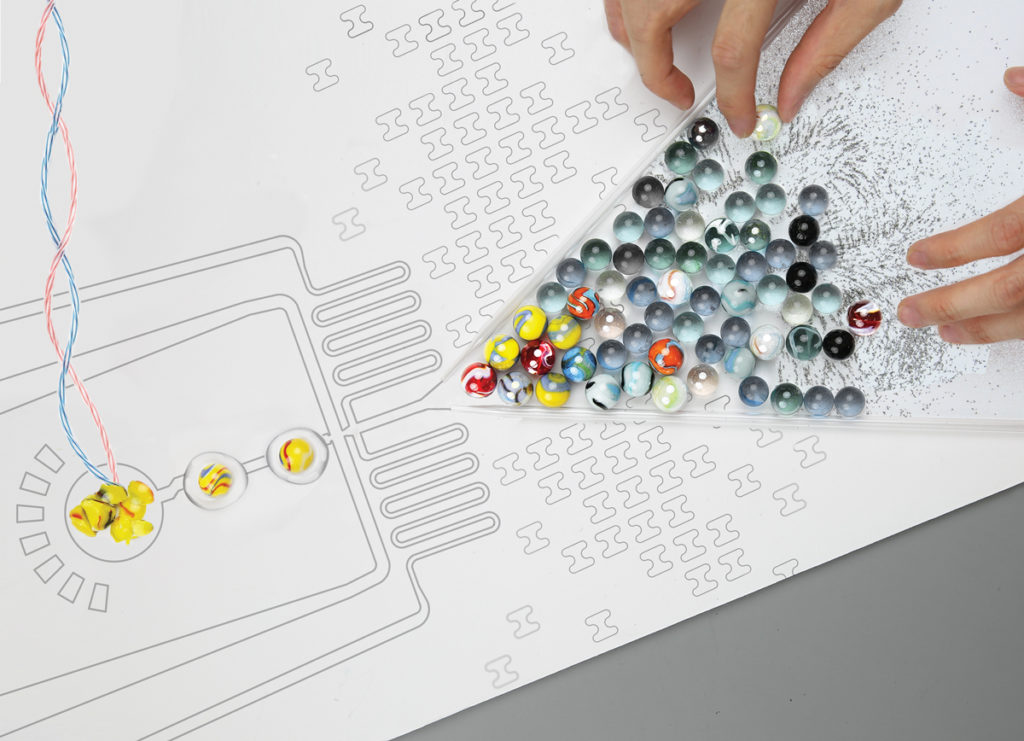
This artistic image represents microfluidic antigen-TCR engagement sequencing, which was highlighted in an article published in the journal Lab on a Chip. This image, created at ISB by Alex Xu, Alphonsus Ng, Allison Kudla and Stella Sun, was featured as cover art by the publication.
Members of ISB’s Heath Lab and their collaborators have developed a way to sensitively detect and analyze neoantigen-specific T-cell populations from tumors and blood. This promising development may have implications for creating targeted, individual-specific cancer vaccines.
The work, detailed in two separate papers, was published in Cell Reports and Lab on a Chip.
The immune system’s T cells monitor diseased cells by recognizing and attacking foreign particles, called antigens, which are presented on molecules called Major Histocompatibility Complexes (MHCs). These antigens can come from viruses, bacteria, or even cancer, allowing the immune system to respond to many threats.
Mighty, yet sparse
However, T cells that target a specific antigen are sparse — often literally one-in-a-million — making them difficult to study. “Naturally occurring antigen-specific T cells are often insufficient to fight off the deadliest diseases,” said Dr. Alphonsus Ng, a postdoctoral fellow at ISB and a lead author on the papers.
ISB researchers engineered MHCs, nanomaterials, and lab-on-a-chip devices to present antigen-presenting MHCs at high densities, magnetically extract T cells that bind MHCs, and count or sequence these T cells.

ISB researchers engineered MHCs, nanomaterials, and lab-on-a-chip devices to present antigen-presenting MHCs at high densities, magnetically extract T cells that bind MHCs, and count or sequence these T cells. The cover art was created at ISB by Drs. Alphonsus Ng, Alex Xu and Allison Kudla.
“If we know which T cells are effective natural defenses — and especially if we can sequence the genes that make them effective — we can better understand and engineer the immune system,” Ng said.
Personalizing immunotherapy
With the ability to count and sequence antigen specific T cells, one can identify the most effective types for fighting diseases, compare those findings to large databases to account for individual patient or community differences, and grow engineered T cells to bolster natural immune defenses and provide new immune capabilities.
“Immunotherapy is one of the most exciting new prospects for cancer treatment. We are combining the strengths of nanomaterials, lab-on-a-chip devices, and computational analysis to search through the haystack of immune cell diversity and find special cancer-fighting T cells,” said Dr. Alex Xu, postdoctoral fellow at ISB and one of the papers’ authors.
“These technologies make cell-based immunotherapy easier to personalize for individual patients by supercharging the search for neoantigen-specific T cells,” said ISB President Dr. Jim Heath. “In fact, the technology was the basis for Pact Pharma, a company that I and some of my co-authors founded a couple of years ago. PACT opened its first clinical trial this past July,” he said.