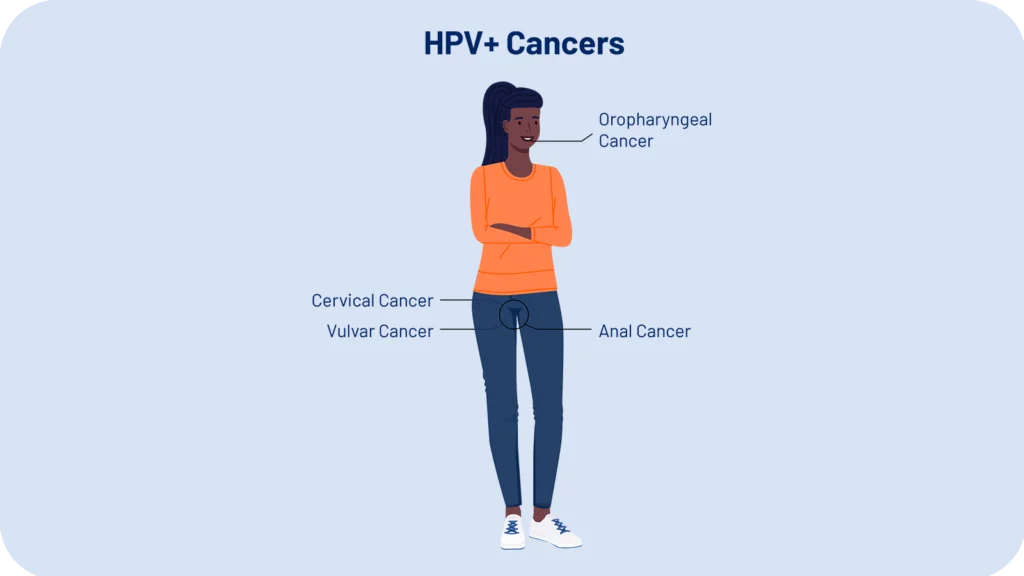
Women’s Health Consortium: Revolutionizing HPV+ Cancer Treatment.
A Collaborative Approach to Engineered T Cell Immunotherapy to Benefit All Women with Advanced HPV+ Cancers.

A purple ribbon, the color for gynecologic cancers, composed with diverse faces illustrated by Stacey Knipe.
Our Background
The Women’s Health Consortium (WHC) is a pioneering collaboration of leading researchers and clinicians dedicated to transforming the treatment of advanced HPV+ malignancies in women. One of the most promising treatments for advanced HPV+ cancers is T cell receptor-engineered T cell immunotherapy. However, only a fraction of patients qualify for this treatment because it requires a specific immunological genetic background.
In 2022, Dr. Jim Heath, president of the Institute for Systems Biology (ISB), brought together a group of physicians and scientists to form the WHC, with the goal of developing cutting-edge engineered T cell immunotherapies designed to treat all patients. Our research focuses on achieving significant improvements in treatment outcomes and quality of life for all women.
We are grateful for the early support we have received from the Andy Hill CARE Fund in Washington state and the National Cancer Institute.

Our Mission
To leverage the power of engineered T cell immunotherapy to eradicate advanced HPV+ cancers, improving the lives of women globally.
Our Approach
The Women’s Health Consortium (WHC) utilizes a multi-faceted approach combining world-renowned talent and innovative technologies.
Collaborative Partnerships
Our team includes leading experts in gynecologic oncology, immunology, and molecular biology, bringing together the collective knowledge and resources of ISB, UCLA, Johns Hopkins Medical, the Swedish Cancer Institute, and the City of Hope Cancer Center, ensuring comprehensive research and swift translation to clinical practice, and allowing us to efficiently design and execute multi-site clinical trials.
Innovative Research Technologies
We have developed high throughput pipelines for the discovery of HPV-targeting T cells, for both cytotoxic (CD8+) and helper (CD4+) T cell classes, and for common HLA alleles for all major ethnicities. We have developed a highly rigorous pre-clinical validation pipeline for advancing those T cells into the clinic. We have further developed non-viral precision cell engineering methods to make cell manufacturing both scalable and significantly more affordable.
Our Growing Library of T cell Receptors
We are developing a library of HPV-specific T cell receptors (TCRs) associated with both cytotoxic (CD8+) and helper (CD4+) T cells. We measure the immunological genetic signatures of potential patients and then use that information to select TCRs from our library to design personalized therapies. Ultimately, we will have 10-12 TCRs in the library, which will enable us to treat almost everyone with a cell therapy built from up to three TCRs.
One TCR in our library has already been shown to be effective in treating patients in a groundbreaking 2021 publication from Christian Henrichs. Our other TCRs have now undergone complete or near-complete pre-clinical validations.
Click on the PDF icons below to see the representative data for TCR1, TCR2, and TCR3-7.
Key Researchers and Clinicians

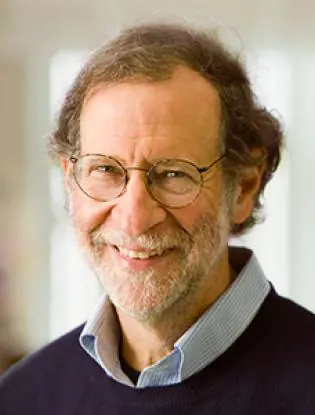
James R. Heath, PhD
President of the Institute for Systems Biology, renowned expert in T cell biology and cancer immunology. Dr. Heath has developed several widely used tools in immuno-oncology and is leading the WHC's efforts to expand access to T cell therapy.

Connie Trimble, MD
Professor of Gynecology and Obstetrics at Johns Hopkins Medical School. Dr. Trimble's expertise lies in non-surgical HPV cancer treatment strategies, using immunotherapy and repurposed plant-derived compounds.

Antoni Ribas, MD, PhD
Professor of medicine at UCLA and Director of the Parker Institute for Cancer Immunotherapy. Dr. Ribas has played an instrumental role in the development of several FDA-approved cancer therapies.

Deborah Wong, MD, PhD
Associate Professor and Director of the Head and Neck Medical Oncology Program at UCLA. Dr. Wong focuses on identifying novel therapeutics and understanding resistance mechanisms for head and neck cancers.

Cristina Puig-Saus, PhD
Assistant Professor at UCLA, focusing on T cell responses to cancer and the development of novel CAR-T cell therapies.

Mihae Song, MD
Assistant Professor at City of Hope, specializing in gynecologic oncology with expertise in minimally invasive surgeries.

Joycelynne Palmer, PhD
Director of the Division of Biostatistics at City of Hope. Dr. Palmer leads the Biostatistics and Mathematical Oncology Shared Resource, providing statistical expertise for basic, translational, and clinical research.

Christine Brown, PhD
Deputy Director of the T Cell Therapeutics Research Laboratory at City of Hope. Dr. Brown provides scientific oversight for preclinical and clinical trial programs focused on engineered T cells.
Stephen Forman, MD
Director of the Hematologic Malignancies Research Institute at City of Hope. Dr. Forman is an international expert in leukemia, lymphoma, and bone marrow transplantation and deeply involved in translational and clinical research.

Kelly Paulson, MD, PhD
Lead, Center for Immuno-Oncology at the Paul G. Allen Research Center. Dr. Paulson integrates cutting-edge science with compassionate care, focusing on skin cancer and solid tumor immunotherapy.

Charles Drescher, MD
Gynecological oncologist specializing in ovarian cancer at Swedish Cancer Institute. Dr. Drescher's work emphasizes prevention and early detection.
WHC Research Contributions and Scientific Publication Links
Our trial will explore a novel approach to treating HPV-associated cancers using personalized cell therapy. We are developing a library of tailored T cell receptors (TCRs) that represent the majority of all ethnicities. Based on a patient’s genetic markers, we will be able to choose the relevant TCRs from the library and personalize a treatment to target their cancer. Learn more about the relevant research that sets the stage for this revolutionary trial below.
Increasing Access to Treatment
We are building on a groundbreaking investigation to treating late-stage HPV+ tumors in Caucasian women of European descent. In a Nature publication, we describe a toolset that is a key technological advancement in building a T cell library that will allow us to treat women of many more ancestries. We describe that technology at a higher level of detail in a Nature Communications Biology publication.
A Fast, Cost-effective, More Precise Treatment
Unlike traditional viral methods that are costly and slow, our non-viral CRISPR-based technique is precise, efficient, and 10 times more affordable. This innovative method for matching and delivering TCRs, proven safe and effective in our recent Nature publication, offers hope for faster, personalized treatment, helping women receive life-saving therapies without the long delays associated with traditional approaches.
Decoding T Cell Receptors
At the heart of our therapy are the T cell receptors that direct cytotoxic and helper T cells to the tumor. Upon tumor encounter, the T cells can function in a myriad of ways, from tumor killing to building tumor memory. We have developed novel experimental and computational pipelines for decoding what anti-tumor properties those T cells will exhibit upon tumor encounter. See this preprint (now accepted to Nature Communications), this Cell Reports paper, and this Cell Systems paper.
Understanding Immunotherapy Resistance
In developing innovative treatments for Merkel cell carcinoma (MCC), a rare and aggressive skin cancer, immunotherapy has shown promise, but many patients develop resistance. As detailed in this Nature Communications paper, tumors suppress HLA genes which help the immune system recognize cancer cells. Recent studies explored gene-engineered T cells and therapies to restore HLA expression, leading to tumor regression in some patients. These findings, published in a preprint, highlight the potential of combining targeted gene therapy and immune-boosting strategies to overcome immunotherapy resistance.
Challenges with HPV Vaccines
In a Lancet Global Health article, Dr. Trimble of the WHC discusses the challenges with HPV vaccines, especially in girls from low-income and middle-income countries, as well as the limitations of HPV vaccines once a girl is already HPV+.
We have designed a multi-site clinical trial in which elements from a library of HPV-targeting T cells are matched to a patient’s specific genetics. Each patient receives up to three separately engineered T cells, enabling us to create a therapy aimed at both tumor eradication and immunological memory to prevent relapse. We are seeking funding to support this trial.
Join us in our journey to bring effective treatments to all women with HPV+ cancers.
You can help us in our mission to transform the treatment of HPV+ cancers in women. Your support will help us bring innovative therapies to patients in need.

Contact Dr. James R. Heath
President and Professor
ISB